WE UNDERSTAND that you might be worried about coronavirus – also known as COVID-19 – particularly if your child has a long-term health condition.
This information sheet from Bradford Teaching Hospitals sets out our advice and the action we are taking to respond to the coronavirus outbreak.
We are following official guidance from the NHS, UK Government and World Health Organisation. The situation is changing constantly so we will update this information as needed – you can also check the GOV.UK website for up-to-the minute advice.
Frequently Asked Questions
What is the coronavirus (COVID-19)?
COVID-19 is a new virus that is spreading across the world. They are very small and look like they have a crown when you look at them using a microscope. This is a virus that affects the lungs and therefore people’s breathing.
What are the symptoms of coronavirus?
- Cough
- High temperature
- Difficulty breathing
However, these symptoms are, of course, similar to lots of other common illnesses. The only way you can be sure if someone has coronavirus is to test them.
Should you be worried?
It is important not to panic. Novel coronavirus (COVID-19) appears to generally cause mild illness in children. So far there have not been many reported cases in children across the world.
If you are concerned, please do not take your child to your doctor or pharmacist – stay at home and call NHS 111 for advice.
What precautions should I take?
COVID-19 is spread by droplets. That means your child needs to be in extremely close contact with someone with COVID-19 (who is coughing) to become infected (within 1-2 metres of them). However, the droplets containing COVID-19 can survive for hours on hard surfaces (door handles, handrails etc). This means that your child is much more likely to get infected by picking up COVID-19 on their hands and then infecting themselves by touching their face (which allows the virus to enter via their mouth, nose or eyes).
 Do
Do
- wash your hands with soap and water often – do this for at least 20 seconds
- use hand sanitiser gel if soap and water are not available
- wash your hands as soon as you get back home
- cover your mouth and nose with a tissue or your sleeve (not your hands) when you cough or sneeze
- put used tissues in the bin immediately and wash your hands afterwards
- limit contact with people if it isn’t necessary
 Don’t
Don’t
- do not touch your eyes, nose or mouth if your hands are not clean
- do not have visitors to your home, including friends and family
Read more on NHS.UK.
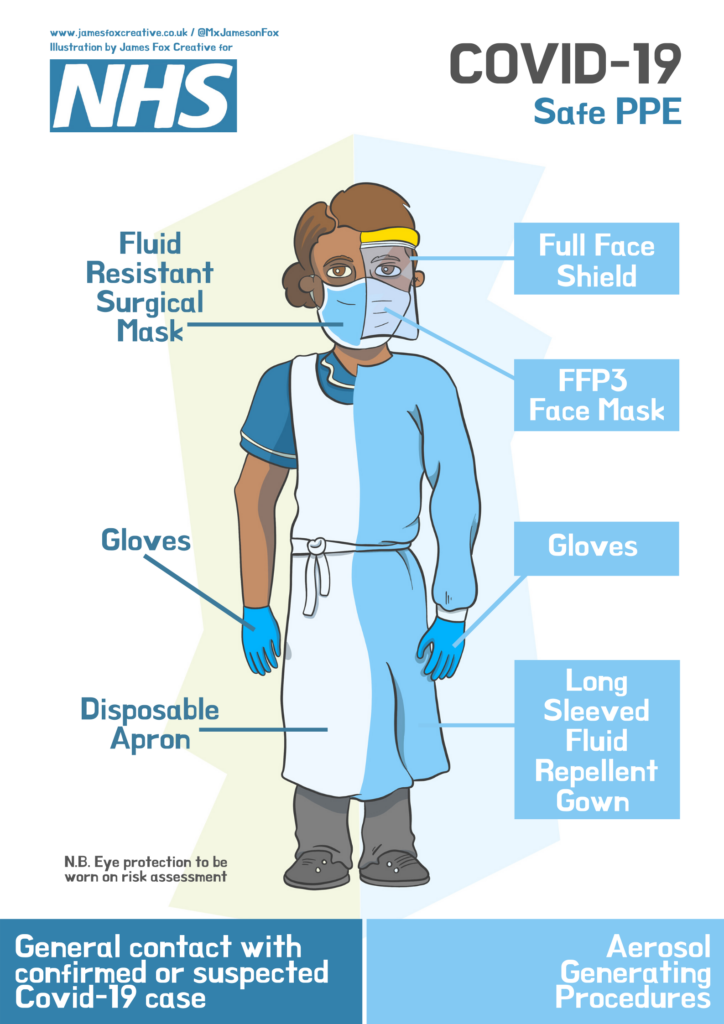
Should we be wearing masks?
Masks are generally not effective, most people do not have appropriate training for a good fit. They also need replacing regularly and there is probably greater risk of contaminating your face from your hands adjusting a mask. Some countries do recommend wearing a mask if a person has coronavirus to help reduce spread; this is not the case in the UK at the moment. The exception is a healthcare setting when you are given a mask, shown how to wear it and it is disposed of appropriately.
What should you do if your child comes into contact with coronavirus?
The incubation period of novel coronavirus is up to 14 days. This means that if your child remains well 14 days after contact with someone with confirmed coronavirus, they have not been infected.
If your child displays symptoms of infection (cough, breathing difficulty or fever) up to 14 days after a contact with someone with confirmed coronavirus, you must go indoors and avoid contact with other people (as you would do with the flu) and contact NHS 111 online or call NHS 111. If your child has moderate breathing difficulty, they will need to be reviewed by a healthcare professional in hospital. NHS 111 will arrange this. If your child has features of severe breathing problems call 999.
If my child is unwell, can I give them ibuprofen?
There is currently no strong evidence that ibuprofen can make coronavirus (COVID-19) worse. But until we have more information, take paracetamol to treat the symptoms of coronavirus. If you are already taking ibuprofen or another non-steroidal anti-inflammatory (NSAID) on the advice of a doctor, do not stop taking it without checking first.
Will my child be tested for coronavirus?
Only children who are admitted to hospital with moderate/severe symptoms of COVID-19 are being tested.
If your child has mild symptoms, your child will not be tested for COVID-19. Instead, your family will be told to self-isolate for 14 days.
Is the process of testing scary for children?
The reason you’ve been brought to the hospital is to test you for a germ that is so small it cannot be seen. We don’t think that it will make you very poorly but we don’t want it to spread to other people. A doctor or nurse will gently swab your nose and throat. It might feel a little uncomfortable but it won’t hurt.
Although the people doing the testing look scary, they are just normal people underneath the funny mask and clothes!
Is there any treatment?
There is no proven treatment for COVID-19, however, there are many clinical trials underway for many different therapies. Vaccines will hopefully provide protection against future outbreaks of COVID-19, though these are still early in the drug development phase and unlikely to be available this year.
What do I say to my child about coronavirus?
There’s a lot of news coverage about the outbreak of COVID-19 and it can be frightening for children. Parents and others who work closely with children should filter information and talk about it in a way that their child can understand.
- Simple reassurance. Remind children that researchers and doctors are learning as much as they can, as quickly as they can, about the virus and are taking steps to keep everyone safe. Reassure your child that it is unlikely they will get seriously ill, and if they do you feel ill you will look after them.
- Give them control. It’s also a great time to remind your children of what they can do to help – washing their hands often, coughing into a tissue or their sleeves, and getting enough sleep.
- Watch for signs of anxiety. Children may not have the words to express their worry, but you may see signs of it. They may get cranky, be clingier, have trouble sleeping, or seem distracted. Keep reassuring them and try to stick to your normal routines.
- Monitor their media. Keep young children away from frightening images they may see on TV, social media, computers, etc. For older children, talk together about what they are hearing on the news and correct any misinformation or rumours you may hear.
- Be a good role model. COVID-19 doesn’t discriminate and neither should we. While COVID-19 started in Wuhan, China, it doesn’t mean that it makes someone more susceptible to the virus or more contagious. Stigma and discrimination hurt everyone by creating fear or anger towards others. When you show empathy and support to those who are ill, your children will too.
Ten tips from YoungMinds.
Will my child's upcoming appointment or admission be cancelled?
In the current situation, we are working hard to ensure we are able to deliver care to those patients who most need our help. If there is a change to your appointment or admission, you will be contacted directly.
If I am visiting my child on the ward am I allowed to bring other children or family members as well?
Visiting is restricted. In the paediatric and neonatal departments, one parent or appropriate adult is able to be with their child at any given time. No other children will be able to visit.
Chronic illness and coronavirus
How might coronavirus affect children with chronic illness and other health conditions?
Fortunately, current information suggests that children are unlikely to become severely ill with the coronavirus (COVID-19). However, children with certain underlying conditions may be at higher risk, specifically those children with problems that impact the heart, lungs or ability to fight infection. Examples of conditions include:
- Chronic lung disease-cystic fibrosis, primary Ciliary Dyskinesia (PCD), bronchiectasis, difficult asthma, oxygen dependant chronic lung disease and tuberculosis
- Children on home ventilator support
- Complex heart disease
- Respiratory complications of neurodisability (including muscle disorders)
- Children considered to have underlying life-limiting illness
- Immunodeficiency conditions
- Organ transplant, lung transplant and bone marrow stem cell transplant
- Current/recent (within six months) cancer chemotherapy/immunotherapy treatment
- Children with inflammatory bowel disease and rheumatologic conditions who are taking medications that lower the immune system
What medications can cause weaken immune system?
Prednisolone, high dose inhaled corticosteroid, cyclosporine, MMF, Gamma interferon, Tacrolimus, sirolimus, Rituximab, Azathioprine, 6- Mercaptopurine, Methotrexate, Infliximab and Adalimumab.
Conditions
Asthma
If your child gets an asthma cough and you are unsure whether your child’s cough is a symptom of COVID-19 or related to asthma, please speak to your GP, use the online 111 service or call 111 to ensure that your child gets the right care.
Keep following the asthma action plan to manage asthma. If your child is having an asthma attack, call 999 for an ambulance as usual, and tell them your child has COVID-19 symptoms.
If your child has severe asthma
Severe asthma is hard to treat, and often the symptoms are not well controlled, even with high doses of medicines.
Having severe asthma is likely to put your child at higher risk of complications from COVID-19; you should follow the advice above, and try to be extra careful about avoiding unnecessary contact with other people.
Read more about managing asthma.
Rheumatological conditions
Is my child / young person specifically at risk as they are on immunosuppressant medication for their Rheumatological condition?
Being on some medications, particularly steroids and /or biologics (such as etanercept / adalimumab / tocilizumab / abatacept / infliximab / rituximab) does cause a greater amount of immunosuppression and therefore may increase risk, although the greatest risk actually comes from being exposed to the virus, which is why the hygiene measures are so important. Many patients are on methotrexate. Whilst this does not cause as much immunosuppression, much of this advice would also apply to them.
 Should my child / young person stop taking medication?
Should my child / young person stop taking medication?
No. Current advice is to continue taking all medication as prescribed. Stopping may cause a flare-up of disease requiring more intensive treatment. Contact your paediatric rheumatology team if your child is currently on steroids for possible dose adjustment.
Inflammatory bowel disease (IBD)
Do all IBD patients have a weakened immune system and what should I do about medication?
Stay on your medication.
- If you are taking a mesalamine, these are all safe and are not immune suppressant medications.
- While taking these medications, you do not need to take extra precautions beyond the recommended personal hygiene.
- If you are taking steroids (prednisone/prednisolone) for any reason, be sure to take extra precautions and talk to your healthcare provider, as steroids can suppress your immune system.
- Immunomodulators like thiopurines (azathioprine, 6-mercaptopurine, cyclosporine, methotrexate) tend to inhibit the body’s immune response to viral infections.
- Do not stop taking these medications. If you have concerns, talk to your provider.
- Biologics/Biosimilars including infliximab are immune suppressing drugs.
- Do not stop taking these medications.
- Talk to your healthcare provider before making any adjustments to these medications.
- If your medication requires an infusion please do not skip these appointments. It’s important to stay on your medication and go to infusion appointments as scheduled. If you have concerns about visiting an infusion centre:
- Talk to your doctors, and discuss your concerns.
Read more about what IBD patients should know.
Primary immunodeficiency
Children who have primary immune deficiency diseases are different from the general population. Some children don’t have a typical fever response to infections.
Chronic lung conditions
Evidence has shown that people with chronic lung conditions including cystic fibrosis and PCD seem to be at greater risk of serious illness from COVID-19.
- Follow the general healthy precautions and social distancing as advised by the Government.
- There is no evidence that wearing surgical masks provides personal protection. However, you may be asked to wear a mask when attending hospital, as this relates to protecting others.
- If you develop cold or ‘flu-like’ symptoms (muscle aches, fever etc), speak with your respiratory team about starting a recommended back-up antibiotic treatment. We advise storing spare dry powder antibiotics or antibiotic tablets at home to start promptly, if needed.
- Stock up on supplies.
Read more from Cystic Fibrosis Trust.
Congenital heart disease
The Government has stated that patients with ‘chronic heart disease’ are likely to be at increased risk of severe illness from coronavirus. While technically all children with heart problems have ‘chronic heart disease’, most are at no greater risk than the general population and the general Government recommendations should be followed.
It is possible that such children might be more at risk of becoming unwell, including patients:
- with a single ventricle, Fontan circulation or Glenn shunt;
- who have cyanosis (low blood oxygen levels);
- who have heart failure/cardiomyopathy requiring medication;
- who take regular medicines to improve heart function;
- with pulmonary hypertension or Eisenmenger syndrome;
- with tetralogy of Fallot, an atrioventricular septal defect or a large ventricular septal defect that has not yet been operated on;
- with Di George syndrome if the immune system is affected.
Read advice from Leeds Congenital Hearts.
Epilepsy
Epilepsy is a “family” of many different disorders that lead to seizures. Some people will have easily controlled seizures, have no other health problems, and become seizure-free on medications. Or they may have epilepsy with occasional seizures but no other health problems. For these people, the available data suggests that just having epilepsy alone
- does not increase the risk of getting COVID-19 and
- does not increase the severity of COVID-19
Some people with epilepsy regardless of seizure control have other health conditions that put them at higher risk from COVID-19. They may be taking medicines to control seizures that also affect their immune system (for example, ACTH, steroids, immunotherapies). Or they may have other neurological or developmental issues that affect their immunity. People in these situations are at greater risk of developing more severe symptoms with viral illnesses.
Read more from Epilepsy Foundation.
Diabetes
Are children with diabetes more likely to develop COVID-19?
Type 1 diabetes in itself is not associated with worse disease in children.